Flashers, Floaters and Retinal Detachment
What are flashes and floaters? What causes them?
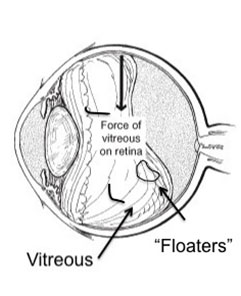
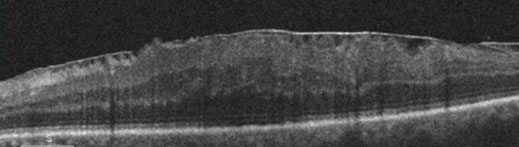
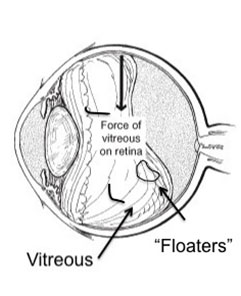
The center of the eye is filled with a clear gel called vitreous. When we are born, the vitreous in both eyes is completely clear and stuck down everywhere to the inside surface of the eye (including the retina). As we get older the gel clumps together – these cast shadows on the retina (light sensing part of the eye) causing the occasional “floaters” we see.
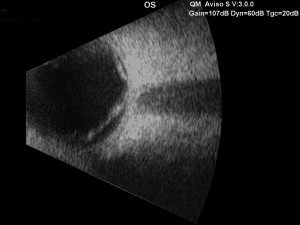
After several decades (usually after age 50) the gel liquefies and starts to separate from the back of the eye. This is called a posterior vitreous separation or detachment. When this occurs a large floater can be seen. People sometimes describe this as “a circle,” “a cobweb,” “a spider,” etc.
As the separation progresses (usually over 4-6 weeks) the gel can tug on the retina (back of the eye). This causes flashes of lights. Though the flashes do not cause damage, a flash could indicate that the gel is pulling especially hard increasing the risk of a tear in the retina.
The appearance of flashes and floaters may be alarming, especially if they develop suddenly. You should contact your eye doctor right away if you suddenly develop new flashes or floaters.
Are floaters ever serious?
The retina can tear if the shrinking vitreous gel pulls away from the wall of the eye. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters. A torn retina is always a serious problem, since it can lead to a retinal detachment.
You should call your eye doctor as soon as possible if:
- Even one new floater appears suddenly
- Lots of “pepper spots” in your vision
- You see sudden flashes of light
- You notice loss of any peripheral (side) vision
How are your eyes examined for flashes and/or floaters?
When an ophthalmologist examines your eyes, your pupils will be dilated with eye drops. During this examination, your ophthalmologist will carefully observe your retina and vitreous using a bright light. Evaluation for retinal tears usually requires a technique called “scleral depression” for which your ophthalmologist will use an instrument to gently press on your eyelids. This office examination is done with minimal discomfort.
Because your eyes have been dilated, you may need to make arrangements for someone to drive you home afterward. Floaters and flashes of light become more common as we grow older. While not all floaters and flashes are serious, you should always have a medical eye examination by an ophthalmologist to make sure there has been no damage to your retina.
What can be done about floaters?
Floaters can get in the way of clear vision, which may be quite annoying, especially if you are trying to read. Though most floaters will always be there, people usually notice them less over time. Floaters can be surgically removed, but this is not performed routinely as most people have minimal symptoms after a couple months. Even if you have had some floaters for years, you should have an eye examination immediately if you notice new ones.
What is a retinal detachment?
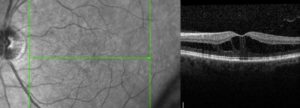
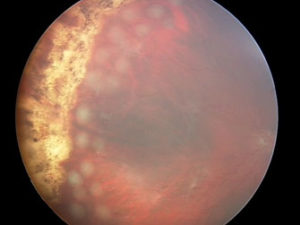
The retina is the sensory tissue that lines the back wall of the eye. It can be described as the wallpaper of the back of your eye. A retinal detachment occurs when the retina is separated from the inside of your eye and can no longer transmit images properly through the optic nerve to the brain. The center of the retina is the macula. If the macula is involved in the detachment, the vision is often extremely blurred. If the macula is not involved in the area of detachment, there may be some loss of peripheral vision.
Is retinal detachment serious?
Yes. A retinal detachment is a very serious problem that will almost always lead to blindness if not treated.
What causes a retinal detachment?
As described above, in some cases vitreous separation can cause a tear (or tears) in the retina. As time passes, fluid from the center of the eye will pass through the tear and begin accumulating beneath the retina, causing a retinal detachment. There are some conditions that increase the likelihood of developing a retinal detachment, including the following:
- Myopia (nearsightedness)
- Traumatic injury
- A history of retinal detachment in either eye
- Family history of retinal detachment
What are the symptoms of a retinal detachment?
- A new floater or several floaters (can be hundreds) that appear suddenly
- Sudden flashes of light in the eye
- Seeing “cobwebs” or hairs in field of vision
- Impression of a curtain or veil coming down over vision (Loss of peripheral, and then central,
vision)
- Blurred vision
- Pain is not a symptom of a detached retina
How is retinal detachment repaired?
A retinal detachment can be repaired in several different ways. The surgery chosen depends on the age of the patient, the type of retinal detachment, whether the patient has had cataract surgery or not, surgeon preference, and other factors. The four general categories of retinal detachment repair are:
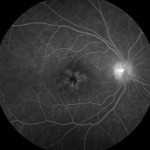
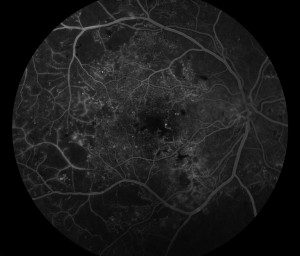
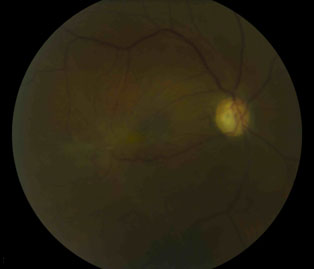
- Laser barricade – does not fix the detachment but prevents it from spreading; can be done in the office).
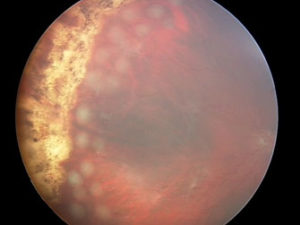
Laser barricade
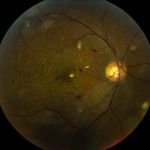
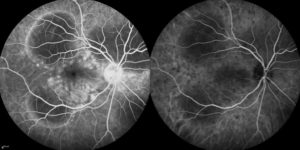
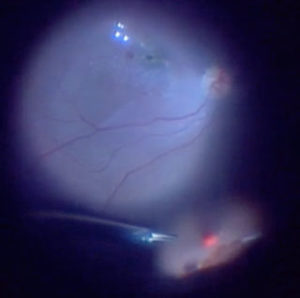
- Pneumatic Retinopexy – a combination of treating the tear with cryotherapy (freezing treatment) or laser and the use of a gas bubble injected into the eye to help the eye get rid of the fluid. The picture shows the injection of a gas bubble that will cover the tear in the retina. This prevents fluid from getting behind the retina and allows the body to absorb the fluid and flatten the retina.
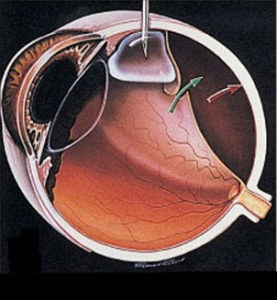
Pneumatic retinopexy
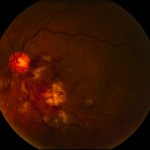
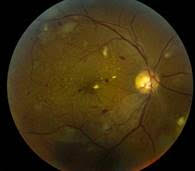
- Scleral Buckle – a scleral buckle involves first treating the tear in the retina with cryotherapy (freezing treatment) and then placing a silicone band under the muscles around the eye to support the tear. The fluid can be drained from under the retina or a gas bubble can be injected into the eye similar to pneumatic retinopexy.

Scleral Buckle
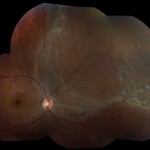
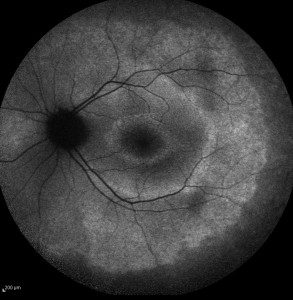
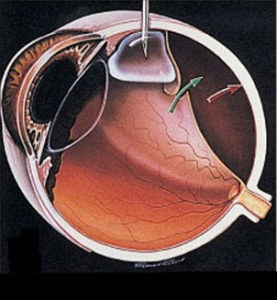
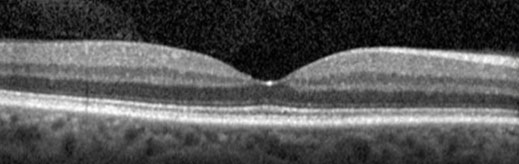
- Vitrectomy – vitrectomy involves the removal of the vitreous (floaters) from the eye using small instruments. This removes all the traction (pulling) on the retinal tear(s) and detachment. The vitreous space is then filled with a long-lasting gas bubble that keeps the retina flat until the tears heal. Laser use used to seal the tear(s).
Vitrectomy
Sometimes both a scleral buckle procedure and vitrectomy are used together to fix complex retinal detachments.
For additional information, download the following forms about:
- Diabetic Retinopathy
- Epiretinal Membrane/Macular Pucker
- Flashes, Floaters and Retinal Detachment