Frequently Asked Questions
GLAUCOMA
What is glaucoma?
Glaucoma is a disease of the optic nerve that is associated with an elevated eye pressure, optic nerve changes, and visual field loss. When a patient has glaucoma, the fluid in the eye does not drain properly causing the pressure in the eye to increase. As the pressure increases, it pushes on the optic nerve causing damage. The damage caused by glaucoma cannot be reversed, however treatments are available to prevent any further vision loss. There are no symptoms of glaucoma, but the loss of peripheral vision can be detected with special testing. It is important to have your eye pressure checked and optic nerve examined yearly.
What causes glaucoma?
There are many causes of glaucoma but the common theme is an increased eye pressure that is associated with a poor drainage system in the eye. It can be associated with increasing age, cataracts, and medical problems like diabetes. There is a strong hereditary component as well.
Who is at risk for glaucoma?
High pressure alone does not mean that you have glaucoma. Your Ophthalmologist considers many factors in determining your risks for developing this disease. The most important risk factors include:
- Age
- Nearsightedness
- African ancestry
- A family history of glaucoma
- Past injuries to the eyes
- A history of severe anemia or shock
Your ophthalmologist will weigh all of these factors before deciding whether you need treatment for glaucoma or whether you should be monitored closely as a glaucoma suspect.This means your risk of developing glaucoma is higher than normal, and you need to have regular examinations to detect the early signs of damage to the optic nerve.
CATARACT
What is a cataract?
A cataract is a clouding of the normally clear lens of the eye. It can be compared to a window that is frosted or yellowed. There are many misconceptions about cataracts. A cataract is not:
- A film over the eye
- Caused by overusing the eyes
- Spread from one eye to the other
- A cause of irreversible blindness
Common symptoms of cataracts include:
- A painless blurring of vision
- Glare or light sensitivity
- Poor night vision
- Double vision in one eye
- Needing brighter light to read
- Fading or yellowing of colors
The amount and pattern of cloudiness within the lens can vary. If the cloudiness is not near the center of the lens, you may not be aware that a cataract is present.
How is a cataract treated?
Surgery is the only way a cataract can be removed. However, if symptoms of a cataract are not bothering you very much, surgery may not be needed. Sometimes a simple change in your eyeglass prescription may be helpful. There are no medications, dietary supplements, or exercises that have been shown to prevent or cure cataracts. Protection from excessive sunlight may help slow the progression of cataracts. Sunglasses that screen out ultraviolet (UV) light rays or regular eyeglasses with a clear, anti-UV coating offer this protection.
Will cataract surgery improve my vision?
The success rate of cataract surgery is excellent. Improved vision is achieved in the majority of patients if other vision-limiting problems are not present.
DIABETIC RETINOPATHY
What is diabetic eye disease?
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of this disease. It is the leading cause of severe vision loss in the working population. It is more common in those with a long history of diabetes and in those patients that have had poor control of his/her blood sugars.
Diabetic eye disease may include:
- Diabetic retinopathy – damage to the blood vessels in the retina.
- Cataract – clouding of the eye’s lens.
- Glaucoma – increase in fluid pressure inside the eye that leads to optic nerve damage and loss of vision.
Cataracts and glaucoma also affect many people who do not have diabetes.
What are the symptoms?
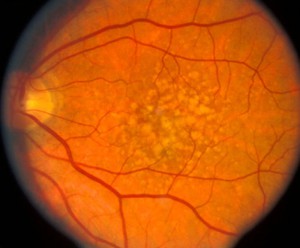
Often there are no symptoms in the early stages of the disease. Vision may not change until the disease becomes severe. Blurred vision may occur when the macula – the part of the retina that provides sharp, central vision – swells from the leaking fluid. This condition is called macular edema. If new vessels have grown on the surface of the retina, they can bleed into the eye, blocking vision. Unfortunately, advanced retinopathy can be present even without vision loss or symptoms and for that reason, an annual exam is recommended.
How is diabetic retinopathy treated?
The best treatment is strict control of your blood sugar. This alone will significantly reduce the long-term risk of vision loss from diabetic retinopathy. If high blood pressure and kidney problems are present, they need to be treated. Laser surgery has been the primary focus of therapy for many years but recently injection therapy has been shown to have superior visual results in some patients. These intraocular injections can cause regression of the hemorrhages, swelling and bleeding that are commonly associated with diabetic retinopathy. Laser still plays a role in treating retinopathy as does more complex vitrectomy surgery for traction retinal detachment and non-clearing vitreous hemorrhages.
What is macular degeneration?
Age related Macular degeneration (AMD) is a leading cause of vision loss in those over 65. The associated anxiety of losing vision and independence can best be addressed with an understanding of the person at risk, the symptoms, and the treatments that improve the prognosis if the diagnosis is made early.