Dr. Christopher Richmond Joins Georgia Eye Institute
June 28, 2023 – Savannah, GA – Georgia Eye Institute (GEI) announces the arrival of Dr. Christopher Richmond to the practice. Dr. Richmond is an Ophthalmologist specializing in cataract and refractive surgery.
Dr. Richmond received his undergraduate degree from Clemson University before attending the University of South Carolina School of Medicine for his doctorate. He completed his internship in General Surgery at Walter Reed National Military Medical Center and his residency in Ophthalmology at the Naval Medical Center San Diego. Dr. Richmond is a member of the American Academy of Ophthalmology and the Society of Military Refractive Surgeons.
Prior to joining Georgia Eye Institute, Dr. Richmond served as an officer and a flight surgeon in the United States Navy. Most recently, he was the Department Head of Ophthalmology at the Naval Hospital in Pensacola, Florida. Dr. Richmond is currently accepting patients at the Savannah campus.
Georgia Eye Institute provides primary care, optical retail locations, and sub-specialty eye care in 11 locations located throughout Southeast Georgia and South Carolina. Subspecialty eye care includes cataract evaluations, retinal care, glaucoma management, functional cosmetic eye surgery, and LASIK laser vision correction.
Dr. Nicolle Oberlin Joins Georgia Eye Institute

April 5, 2022 – Savannah, GA – Georgia Eye Institute (GEI) announces the arrival of Nicolle Oberlin to the staff. Oberlin is an Optometrist with special interests in primary care, including pediatrics and disease, as well as military optometry.
Oberlin received her Bachelor of Science-Vision Science degree and her Doctor of Optometry degree from the College of Optometry at Ferris State University, in Big Rapids, Michigan. She is an active member of the Armed Forces Optometric Association, Michigan Optometric Association, and the American Optometric Association.
Oberlin has previously done an externship at a Special Needs Vision Clinic in Michigan, and most recently was active-duty Assistant Chief of Optometry at Winn Army Community Hospital in Fort Stewart, Georgia. She is now accepting patients in the Hinesville location.
Georgia Eye Institute provides primary care, optical retail locations, and sub-specialty eye care in 12 locations located throughout Southeast Georgia and South Carolina. Our subspecialty eye care includes cataract evaluations, retinal care, glaucoma management, functional cosmetic eye surgery, and LASIK laser vision correction.
Dr. William Degenhart Receives Beacon of Hope Award from Georgia Lions Lighthouse


October 19, 2018 – Savannah, GA – Dr. William Degenhart, board-certified ophthalmologist and founding partner of Georgia Eye Institute, received the Georgia Lions Lighthouse Beacon of Hope Award last night at their annual Evening in the End Zone event held in Atlanta.
The Georgia Lions Lighthouse Beacon of Hope Award honors a medical professional who demonstrates an unwavering commitment to vision or hearing care for the uninsured in his or her community. Dr. Degenhart has been providing eye care since 1982 and his volunteer efforts and support of those in need throughout Savannah and Southeast Georgia continue to inspire and encourage many.
Georgia Eye Institute provides primary eye care, optical retail locations and sub-specialty eye care in 13 locations conveniently located throughout Southeast Georgia and the South Carolina. The sub-specialty eye care includes cataract evaluation and management, retinal care, glaucoma management, functional cosmetic eye surgery and LASIK laser vision correction.
Dr. Thomas James Kandl Joins Georgia Eye Institute

September 6, 2018 – Savannah, GA – Georgia Eye Institute (GEI) announces the addition of Dr. Thomas James Kandl to their staff. Kandl has completed a fellowship in Ophthalmic Plastic and Reconstructive Surgery at the MD Anderson Cancer Center in Houston, Texas. He is seeing patients at the main office in Savannah and specializes in Oculoplastics and Reconstructive Surgery.
Kandl received a Bachelor of Science Degree from Wofford College; a Doctor of Medicine Degree from the Medical University of South Carolina; and was awarded a Doctor of Ophthalmology Degree from Rutgers University.
Georgia Eye Institute provides primary eye care, optical retail locations and sub-specialty eye care in 13 locations conveniently located throughout Southeast Georgia and the South Carolina. The sub-specialty eye care includes cataract evaluation and management, retinal care, glaucoma management, functional cosmetic eye surgery and LASIK laser vision correction.
Georgia Eye Institute is Working To Promote Eye Exams in Southeast Georgia and the Low Country
May 2018 – Millions of people in the United States have undetected vision problems that can cause vision loss and even blindness. Unfortunately, many eye diseases have no early warnings signs or symptoms so you may be affected without even noticing it. Visiting your eye care professional for a comprehensive dilated eye exam is the only way to know if your vision is at its best and your eyes are healthy.
A comprehensive dilated eye exam is a painless procedure in which drops are placed in your eyes to dilate, or widen, the pupil. This allows your eye care professional get a good look at the back of your eyes and examine them for any signs of damage or disease. Georgia Eye Institute recommends that you put a visit to your eye care professional on your “to do” list. Detecting eye diseases in their early stages can help save your sight.
Comprehensive dilated eye exams are important for maintaining good eye health. Healthy vision can help keep you safe when you are behind the wheel, while you are participating in sports, or during recreational activities. It can also help you perform your best on the job and ensure that you maintain a healthy and active lifestyle well into your golden years.
Take care of your eyes and they will help take care of you. Find a window of time to schedule an eye exam today.
Dr. Shari Carney Joins Georgia Eye Institute

28 February 2017 – Savannah, GA – Georgia Eye Institute (GEI) announces the addition of Dr. Shari A. Carney to their staff. Carney, a medical ophthalmologist, will begin seeing patients at the main campus of GEI on February 19th.
Carney received a Bachelor of Science Degree from Clarkson University and a Doctorate of Medicine from Upstate Medical University where she was later Chief Resident in Ophthalmology. Most recently, she was Clinical Assistant Professor of Medical Education for Mercer University School of Medicine, at Memorial University Medical Center. She is a member of the American Academy of Ophthalmology.
Georgia Eye Institute provides primary eye care, optical retail locations and sub-specialty eye care in 13 locations conveniently located throughout Southeast Georgia and the South Carolina. The sub-specialty eye care includes cataract evaluation and management, retinal care, glaucoma management, functional cosmetic eye surgery and LASIK laser vision correction. For more information, visit gaeyeinstitute.com.
Eye Safety for the Solar Eclipse
By Mark Manocha, M.D.
During August 21st’s solar eclipse, it is important to take the proper ocular safety precautions. Looking directly at the sun is never a good idea, so there are a few ways to view it and minimize risk. Savannah will only experience a partial solar eclipse (around 90%), but you can look online to see where totality occurs.
- At no point in Savannah will it be safe to look directly at the sun because it will never be fully covered. Even when the sun is partially covered, it is just as bright, and is equally unsafe.
- Put on your glasses immediately after the sun emerges as looking at it directly, however brief, can cause long-term retinal damage.
- Make sure to look away from the sun before putting on and removing your protective glasses; rapid adjustment to light can also cause severe eye damage.
- You can purchase specially certified glasses (ISO 12312-2) for viewing, which you can find online or in certain stores.
- Regular sunglasses, cameras, binoculars, and telescopes are not safe for viewing the eclipse.
- Alternatively, you can use the pinhole method to project an image of the eclipse on another material. You can do this by poking a hole in a piece of cardboard, and putting a piece of paper behind it, changing the distance until the image is projected clearly onto it.
The solar eclipse is one of the greatest events nature can offer, and it happens rarely in United States. Don’t let this opportunity to witness history pass you by, but make sure to be safe and protect your eyes while viewing this grand spectacle.
Basics of Glaucoma
More than 3 million people in the U.S. have glaucoma. Glaucoma is a complicated eye disease in which the optic nerve gets damaged due to high eye pressure. If it’s not treated properly or is ignored glaucoma can lead to progressive, irreversible loss of vision. Glaucoma is the second most common cause of blindness in the world today.
Glaucoma is incurable, but it can be managed through drug therapies. However, when medication fails to lower the eye pressure, or causes severe side effects, surgery is recommended. In some cases, doctors might recommend surgery as the first course of treatment.
Glaucoma surgery is typically categorized two ways: laser surgery; and incisional surgery. Your ophthalmologist will take into consideration the type of glaucoma you have, its severity, and your general eye health before deciding which type of surgery is most suitable for your condition.
Surgery can stabilize vision by lowering the eye pressure, but it cannot cure glaucoma or reverse any loss of vision which has already occurred.
The following is a brief overview of glaucoma laser surgery and incisional surgery, and what to expect during recovery.
Laser Surgery
Doctors ordinarily recommend laser surgery unless pressure in the eye is extremely high or the damage to the optic nerve is severe.
During this procedure, the eye surgeon improves the drainage system of the eye using a highly focused beam of light. The patient feels no pain during the surgery, as the eye is numbed. A special lens is held to the eye and the laser beam is directed into it.
Immediately after the surgery you may experience blurry vision and some irritation of the eye. Many patients are able to resume normal activities within a day or two after the surgery. However, most doctors recommend patients not lift anything heavy, refrain for any strenuous activity, or do any significant bending for at least two weeks.
Incisional Surgery
Your eye doctor may recommend incisional surgery for any of the following three conditions:
- Extremely high eye pressure
- A severely damaged optic nerve
- Failure to lower eye pressure with laser surgery
During incisional surgery, a small drainage hole is made in the sclera to allow intraocular fluid to bypass the clogged drainage canals and allow the fluid flow from the eye, helping reduce eye pressure.
Shortly after incisional surgery, patients may experience irritation, redness, and increased watering or tearing. Recovery time for incisional surgery is typically longer as compared to laser surgery. Most patients recover in two to four weeks. In some cases, however, recovery time might be longer – up to 2 months.
For more information please call 912.354.4800.
Summer Eye Safety
Summertime means spending more time outdoors, at the beach or pool, and more time in the sun. Most people associate more time in the sun with applying sunscreen to protect the skin, but it’s equally as important to protect your eyes, as exposure to harmful sunlight can lead in an increased risk for eye diseases, including cataract, growths on the eye, and even cancer.
In addition to benefitting your vision health, taking precautionary measures to protect your eyes can also make summertime more fun. Follow these simple tips from Georgia Eye Institute and you and your family can enjoy the summer sun safely while protecting your vision.
Sunglasses are more than just a great accessory
Sunglasses not only look great, they can help protect your eyes from harmful UV rays and reduce the chances of burning your corneas. Sunglasses should fit snugly around your eyes and offer protection on the side of the eyes as well. Keep in mind that sunlight is strongest mid-day, at higher altitudes, and when reflected off water or sand.
Choose sunglasses labeled “100% UV protection,” and only use glasses that block both UVA and UVB rays. It’s important to note that even if you wear UV blocking contact lenses, you still need to wear proper sunglasses to fully protect your eyes.
For maximum protection, wear a hat along with your sunglasses. Broad-brimmed hats are best.
Wear eye protection
Warm, sunny weather means it’s the perfect time for yardwork or to make a dent in your long list of home improvement projects. While doing work on your yard or home, it is extremely important to protect your eyes from dust, dirt and flying debris. Safety goggles can be purchased at home improvement stores, and do a better job of protecting your eyes than sunglasses.
Swim with goggles
Nothing says summer like a day at the beach or the pool. The chlorine in most swimming pools can be particularly irritating to the eyes, causing minor infections and dryness. Salt water from the ocean, rivers other natural bodies of water also contain contaminants that may be harmful to eyes. Wear swim goggles when you’re in the water to protect your eyes from irritants and floating particles that could damage your eyes.
Don’t forget the little ones
While it’s best to keep children out of direct sunlight during the middle of the day, they should wear sunglasses and hats to protect their eyes whenever they’re in the sun, and goggles when they’re swimming.
Eat right for your sight
Nutrition plays an important role in preventing conditions such as cataracts and macular degeneration. A healthy diet of summer foods like strawberries, tomatoes, avocadoes and peppers can help protect your eyes from many common eye conditions. Vitamins C, E and zinc have been shown to slow the aging process in eyes.
Drinking plenty of water can also help keep your eyes healthy. During summer months, it’s easier to become dehydrated, which can cause vision problems. Drink plenty of water to help keep your eyes healthy.
Year-round care
Eyes can be damaged by the sun – even through clouds and haze- any time of year so be sure to give your eyes the same protection year ‘round.
In addition to protecting your eyes in summer, annual visits for your eyes are important and beneficial for your overall health. A thorough eye exam – which is not the same as having a “vision test” – performed by an optometrist or ophthalmologist can detect potentially harmful diseases like diabetes, cardiovascular disease, thyroid disorders and cancers, vision disorders, and issues with the muscles in your eyes.
Georgia Eye Institute provides leading edge primary eye care, corrective eye surgery, ophthalmic care, and surgical eye care at 13 area offices. For more than 20 years the pioneering surgeons and staff at GEI have set new standards for outpatient cataract surgery and lens implantation, offers advanced retinal care for diabetic eye disease, LASIK laser vision correction, glaucoma management, treatment for macular degeneration and corneal disease, oculoplastic surgery, and optometry. For more information, visit gaeyeinstitute.com.
Diabetic Retinopathy FAQs
What is diabetic retinopathy?
Long-standing diabetic disease (in Type I or Type II diabetics) can lead to changes in the back of the eye that can cause a decrease in vision. Specifically, high blood sugar causes damage to the small blood vessels in the retina (layer at the back of the eye that sense light). This damage leads to multiple changes to the retina, especially to the macula, which is responsible for central vision (Figure 1).
What are the different types?
There are two main types of diabetic retinopathy – “Non proliferative Diabetic Retinopathy” and “Proliferative Diabetic Retinopathy.” Proliferative indicates that new, abnormal blood vessels are growing inside the eye, which can lead to bleeding, retinal detachment, and high pressure (all leading to vision loss). Proliferative disease is more sever, but legal blindness can be caused by changes from non-proliferative disease.
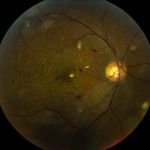
Figure 1 – Normal Macula (the central part of the retina responsible for central vision)
Why do people lose vision from diabetic retinopathy?
Diabetes can lead to vision loss for many reasons, including:
- Swelling in the center part of the vision (Macular edema)
- Loss of blood flow to the center part of the vision (Macular ischemia)
- Bleeding into the central part of the eye (Vitreous hemorrhage)
- Detachment of the back layer of the eye from scar tissue (Retinal detachment)
How is it diagnosed?
The retina can be visualized during a routine eye exam after dilation of the pupil (Figure 3). Optical coherence tomography is a type of non-invasive imaging that allows your physician to view the macula and macular edema (if present) in cross-section (Figures 3 and 4). This is useful for following the disease over time.
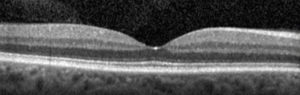
Cross sectional image (Optical Coherence Tomography, or OCT) of a normal macula. The “dip” in the center is the very center part of the vision, or the “fovea.” This is the “20/20? portion of the vision.
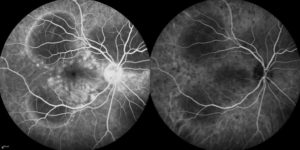
Figure 5. Photograph of the retina (angiogram) that shows loss of blood flow (dark areas).
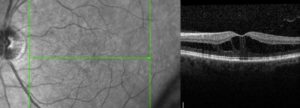
Figure 4. Cross sectional image (OCT) of a macula with diabetic macular edema. Notice the loss of the “dip” and black spaces in the retina. The retina is also thicker because of the swelling. This thickening leads to decreased vision.
How is it treated?
Treatment of diabetic retinopathy depends on the type of disease present. Good blood glucose and blood pressure control are essential in stabilizing disease.
Macular Edema
Edema that affects the center part of the vision is initially treated with medication that is injected into the eye (Figure 6). There are several medications available (Avastin, Lucentis, Eylea, Osurdex implant, steroid). For certain types of edema laser may be used. Laser can be used to destroy leaking blood vessels. A newer technology (micropulse laser) uses non-destructive energy to cause the macula to release factors that cause vessels to stop leaking.
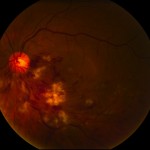
Figure 6. After the surface of the eye is anesthetized (numbed), a small amount of medication is injected into the middle of the eye (vitreous).
Proliferative Diabetic Retinopathy
Proliferative disease (especially if associated with bleeding [vitreous hemorrhage]) is generally treated with laser (panretinal photocoagulation). Laser is used to destroy sick tissue (areas in the back of the eye with loss of blood flow) – this causes abnormal blood vessels to shrink/resolve (Figure 7).
Vitreous Hemorrhage and Traction Retinal Detachment
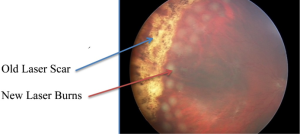
Figure 7. Photo of the retina shows vitreous hemorrhage covering the macula (center of vision) which blurs the vision. Laser scar can be seen peripheral to the blood. This patient required vitrectomy (surgery) to remove the blood.
Proliferative disease that is untreated will lead to bleeding and retinal detachment. The blood itself will usually not harm the eye and will often resolve spontaneously. If the blood does not resolve or if there is retinal detachment that treats the macula (center part of the vision), surgery (vitrectomy) is necessary,. This surgery is performed in an operating room. Small instruments are introduced through micro-cannulas. One instrument provides light and the other instruments to remove blood and scar tissue and place additional laser (Figure 8).
When should a diabetic have a complete eye exam?
A type I diabetic should have their eyes examined within 3-5 years after diagnosis and yearly thereafter if no eye disease is found. A type II diabetic should have their eyes examined at the time of diagnosis and yearly thereafter if no eye disease is found. If diabetic retinopathy is present, follow-up and treatment depends on the severity of the disease or any other issues you may have.

Removal of the vitreous from inside the eye using the “vitrector” (left side of picture). A small instrument (right side of picture) provides the light to see inside the eye. This is done under a microscope.