You should call your eye doctor as soon as possible if:
- Even one new floater appears suddenly
- Lots of “pepper spots” in your vision
- You see sudden flashes of light
- You notice loss of any peripheral (side) vision
How are your eyes examined for flashes and/or floaters?
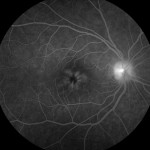
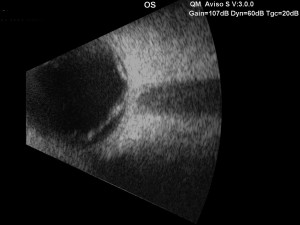
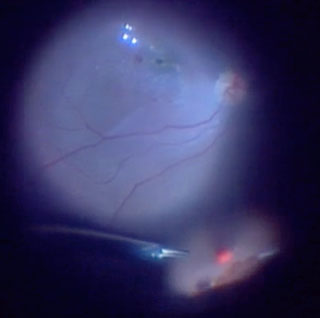
When an ophthalmologist examines your eyes, your pupils will be dilated with eye drops. During this examination, your ophthalmologist will carefully observe your retina and vitreous using a bright light. Evaluation for retinal tears usually requires a technique called “scleral depression” for which your ophthalmologist will use an instrument to gently press on your eyelids. This office examination is done with minimal discomfort.
Because your eyes have been dilated, you may need to make arrangements for someone to drive you home afterwards. Floaters and flashes of light become more common as we grow older. While not all floaters and flashes are serious, you should always have a medical eye examination by an ophthalmologist to make sure there has been no damage to your retina.
What can be done about floaters?
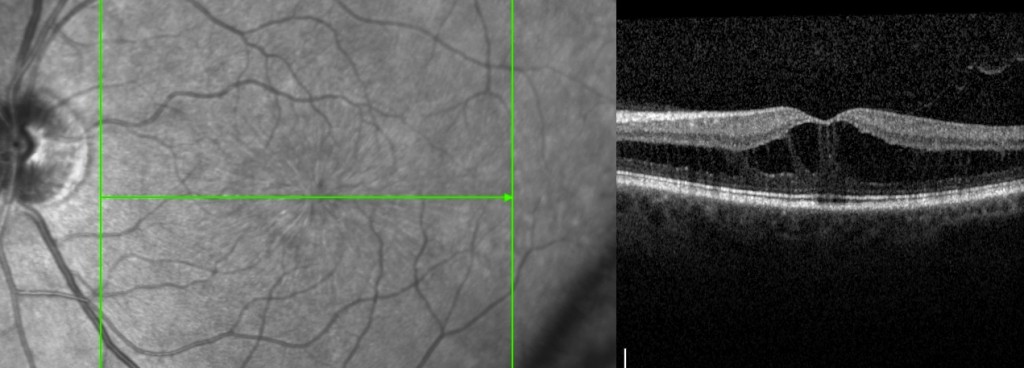
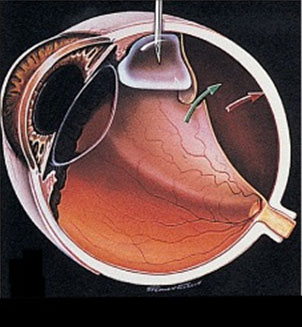
Floaters can get in the way of clear vision, which may be quite annoying, especially if you are trying to read. Though most floaters will always be there, people usually notice them less over time. Floaters can be surgically removed (with surgery called vitrectomy – Figure 3), but this is not performed routinely as most people have minimal symptoms after a couple months. Even if you have had some floaters for years, you should have an eye examination immediately if you notice new ones.
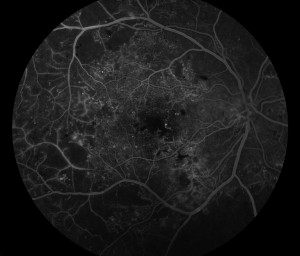
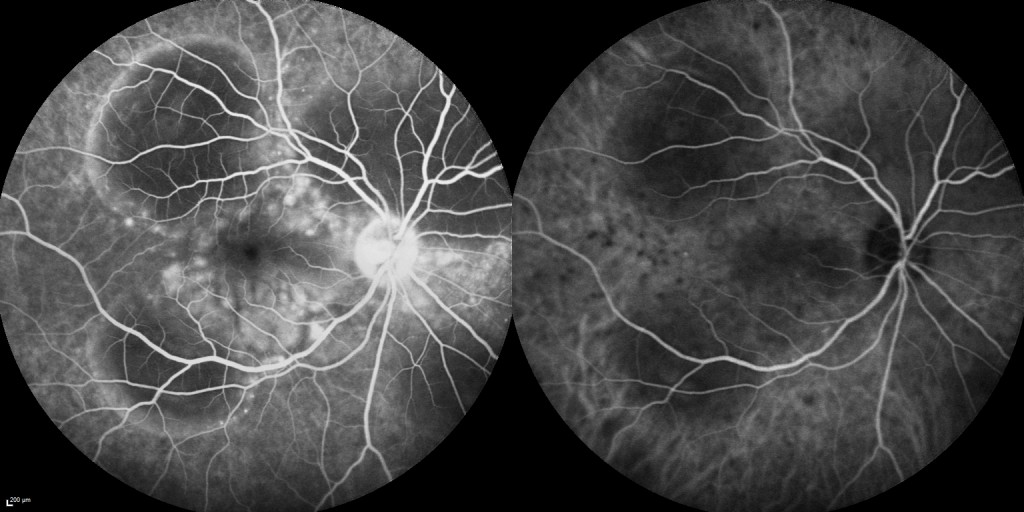
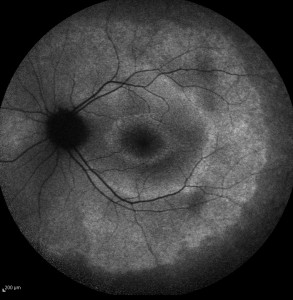
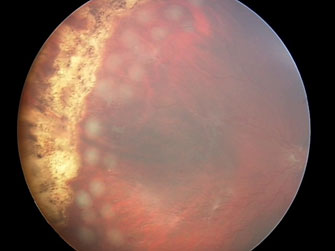
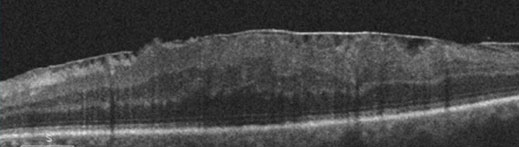
What is a retinal detachment?
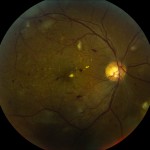
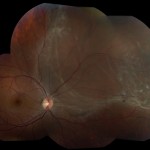
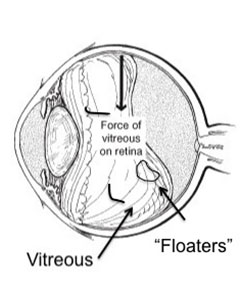
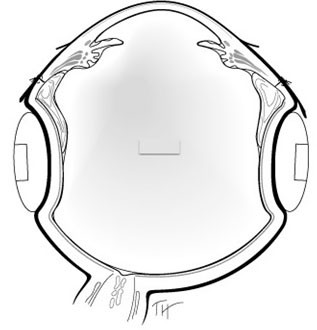
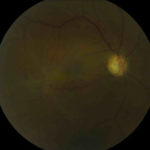
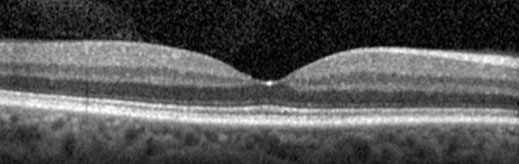
The retina is the sensory tissue that lines the back wall of the eye. It can be described as the wallpaper of the back of your eye. A retinal detachment occurs when the retina is separated from the inside of your eye and can no longer transmit images properly through the optic nerve to the brain. The center of the retina is the macula. If the macula is involved in the detachment, the vision is often extremely blurred. If the macula is not involved in the area of detachment, there may be some loss of peripheral vision.
Is retinal detachment serious?
Yes. A retinal detachment is a very serious problem that will almost always lead to blindness if not treated.
What causes a retinal detachment?
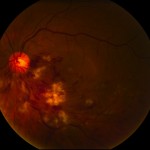
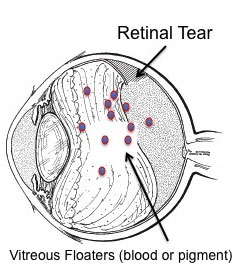
As described above, in some cases vitreous separation can cause a tear (or tears) in the retina. As time passes, fluid from the center of the eye will pass through the tear and begin accumulating beneath the retina, causing a retinal detachment. There are some conditions that increase the likelihood of developing a retinal detachment.
These include:
• Myopia (nearsightedness)
• Traumatic injury
• A history of retinal detachment in either eye
• Family history of retinal detachment
What are the symptoms of a retinal detachment?
• A new floater or several floaters (can be hundreds) that appear suddenly
• Sudden flashes of light in the eye
• Seeing “cobwebs” or hairs in field of vision
• Impression of a curtain or veil coming down over vision (Loss of peripheral, and then central,
vision)
• Blurred vision
• Pain is not a symptom of a detached retina
How is retinal detachment repaired?
A retinal detachment can be repaired in several different ways. The surgery chosen depends on the age of the patient, the type of retinal detachment, whether the patient has had cataract surgery or not, surgeon preference, and other factors. The four general categories of retinal detachment repair are: